You know that![]() sinking feeling you get when something goes wrong? Or how your stomach tightens when you’re feeling angry? What about when you get butterflies in your stomach when you’re thinking about someone you love or something you’re nervous about? Turns out, there’s growing research to show that the gut and the brain are more connected than we previously realized. Improving gut health may even help decrease anxiety and depression, aid in sleep, concentration, and other cognitive functions.
sinking feeling you get when something goes wrong? Or how your stomach tightens when you’re feeling angry? What about when you get butterflies in your stomach when you’re thinking about someone you love or something you’re nervous about? Turns out, there’s growing research to show that the gut and the brain are more connected than we previously realized. Improving gut health may even help decrease anxiety and depression, aid in sleep, concentration, and other cognitive functions.
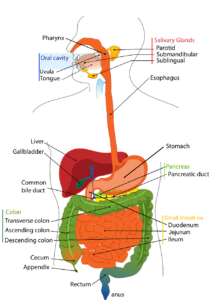
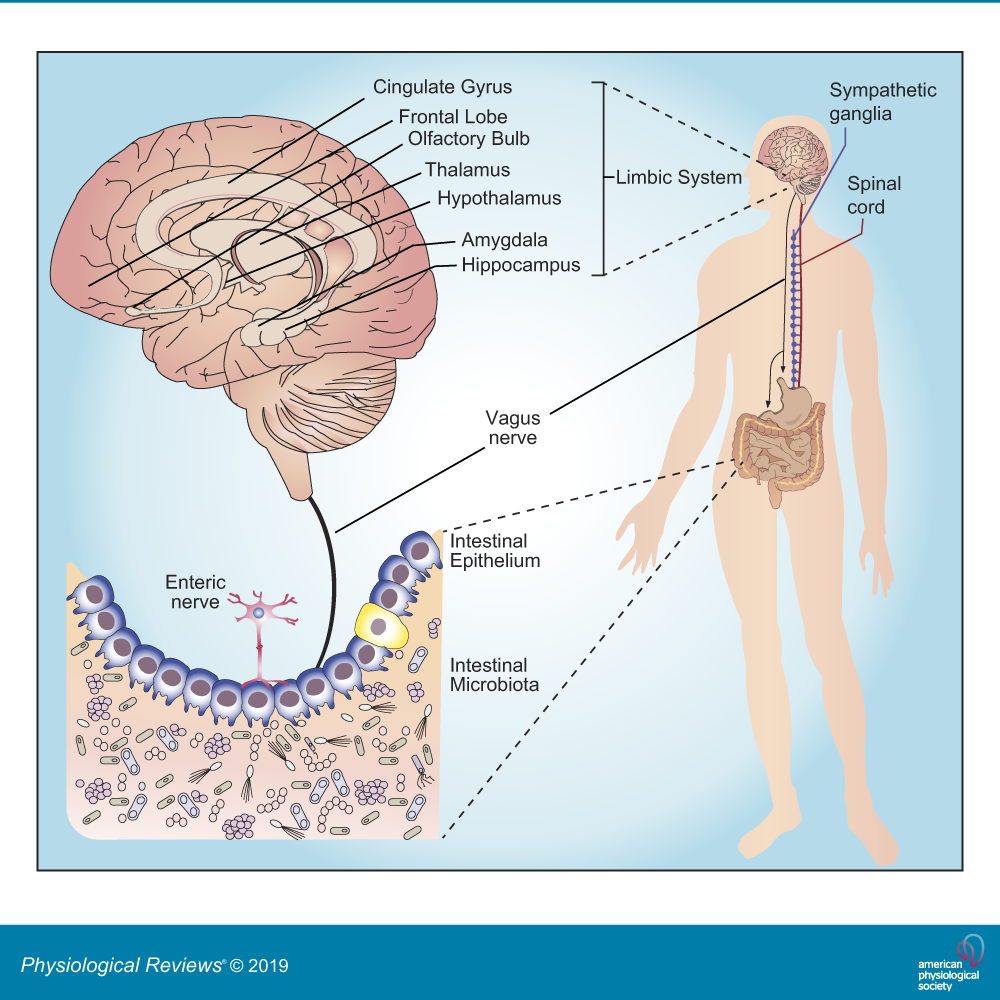
Science is emerging with more evidence of microbiota (the trillions of microorganisms within and on our bodies) which are responsible for regulating gut-brain function. The microbiota-gut-brain axis is the point where the microbiota and the brain communicate with each other through the immune system, tryptophan metabolism, the ![]()
![]()
![]() vagus nerve, and the enteric nervous system (ENS). This is providing researchers and scientists with information regarding the connection between our biological and physiological impact on psychiatric, neurodevelopmental, age-related, and neurodegenerative disorders. While this concept is relatively new, research is showing connections between gut health and Autism Spectrum Disorder, Major Depressive Disorder, Anxiety, Schizophrenia, Bipolar Disorder, Anorexia Nervosa and Cachexia, addiction, ADHD, PTSD, OCD, as well as physical health conditions such as obesity, IBS, etc. This article is going to focus primarily on the mental health relationship to gut health.
vagus nerve, and the enteric nervous system (ENS). This is providing researchers and scientists with information regarding the connection between our biological and physiological impact on psychiatric, neurodevelopmental, age-related, and neurodegenerative disorders. While this concept is relatively new, research is showing connections between gut health and Autism Spectrum Disorder, Major Depressive Disorder, Anxiety, Schizophrenia, Bipolar Disorder, Anorexia Nervosa and Cachexia, addiction, ADHD, PTSD, OCD, as well as physical health conditions such as obesity, IBS, etc. This article is going to focus primarily on the mental health relationship to gut health.
Let me start off by again repeating that more studies need to be done to get a clearer, more well-rounded picture of what’s happening between gut health and mental health. One clear connection between gut health and mental health is the impact of the fight-or-flight response, or the stress response, on the body. We can get activated by our fight-or-flight response several times a day, all day long. Things like deadlines, finances, difficult conversations, traffic, etc. are all day-to-day activities that increase stress and activate this response. When we’re in our fight-or-flight response, our sympathetic nervous system sends messages to the body to prepare us to fight (which can look like anger), flight (which looks like anxiety), and freeze (looks like depression). Several things in the body change as a result of this response. As it pertains to gut health, when we’re in this stress response, our digestive system shuts down and inflammation increases. Once we calm down and are in our parasympathetic nervous system, the digestive processes run smoothly and inflammation is reduced. Many of us, particularly those with mood disorders like anxiety, depression, bipolar, etc., find ourselves getting activated by our stress response several times a day, all day long. This causes our digestive system to turn on and off and on and off all day, wreaking havoc on our bodies. Living with chronic mood disorders can cause long-term impacts on physical health, leading to things like Irritable Bowl Syndrome (IBS) for instance. This is one of those chicken-and-the-egg situations- are those with IBS more likely to develop anxiety? Or does anxiety lead to IBS? Research is expanding to figure out the answers to this.
![]()
![]()
![]()
 Another aspect of this relates to food sensitivities. Each of our bodies responds to food differently. Some people have sensitivities to diary, gluten, food coloring, preservatives, etc. When people eat foods they’re sensitive too, their digestive system attacks that substance- influencing inflammation and our immune system. People have reported that eliminating certain foods from their diet has helped them decrease anxious and depressive symptoms. It may be worth seeing your doctor and having a food sensitivity test completed to see what your system may be sensitive to. This is a very simplified explanation of scientific data, more information can be found at the links below.
Another aspect of this relates to food sensitivities. Each of our bodies responds to food differently. Some people have sensitivities to diary, gluten, food coloring, preservatives, etc. When people eat foods they’re sensitive too, their digestive system attacks that substance- influencing inflammation and our immune system. People have reported that eliminating certain foods from their diet has helped them decrease anxious and depressive symptoms. It may be worth seeing your doctor and having a food sensitivity test completed to see what your system may be sensitive to. This is a very simplified explanation of scientific data, more information can be found at the links below.
Improving gut health can be complicated and, again, more research is needed. For the time being, it appears that monitoring your diet to avoid certain sensitivities, eating mindfully, and reducing stress can all help with gut health and therefore, improve mental health functioning as well. These are all very new and exciting areas to explore and it’ll be interesting to see how this will change, and hopefully improve, healthcare providers’ (mental health and physical health) understanding of the various factors influencing physical and mental health so these conditions can be treated more effectively.
About the Author
Maria Mangione (she/her), M.A., LPCC is a licensed clinical counselor that specializes in dialectical behavior therapy. Maria works to help people develop the tools they need to develop trust in themselves and build their life worth living. Maria believes in having meaningful connections wi ![]() th her clients and believes that therapy and healing can be fun. Click Here to learn more about Maria’s experience and therapeutic style.
th her clients and believes that therapy and healing can be fun. Click Here to learn more about Maria’s experience and therapeutic style.
More information can be found at:
Cryan JF, O’Riordan KJ, Cowan CSM, Sandhu KV, Bastiaanssen TFS, Boehme M, Codagnone MG, Cussotto S, Fulling C, Golubeva AV, Guzzetta KE, Jaggar M, Long-Smith CM, Lyte JM, Martin JA, Molinero-Perez A, Moloney G, Morelli E, Morillas E, O’Connor R, Cruz-Pereira JS, Peterson VL, Rea K, Ritz NL, Sherwin E, Spichak S, Teichman EM, van de Wouw M, Ventura-Silva AP, Wallace-Fitzsimons SE, Hyland N, Clarke G, Dinan TG. The Microbiota-Gut-Brain Axis. Physiol Rev. 2019 Oct 1;99(4):1877-2013. doi: 10.1152/physrev.00018.2018. PMID: 31460832.